Key Takeaways
- Compression socks are typically recommended for daytime wear (8-10 hours) rather than 24/7 use
- Continuous 24/7 wear may be prescribed in specific medical situations
- Proper application and removal are essential for effectiveness and safety
- Graduated compression (tightest at ankle, looser up the leg) improves circulation
- Regular breaks allow skin to breathe and reduce risk of complications
- Consult healthcare providers before wearing compression socks around the clock
- Different compression levels (8-40+ mmHg) serve different therapeutic purposes
- Proper sizing is critical for both comfort and medical effectiveness
- Quality compression garments should be replaced every 3-6 months with regular use
- Alternative compression strategies may provide benefits without continuous wear
Understanding Compression Socks and Their Purpose
Compression socks are specialized garments designed to improve blood circulation in the legs by applying graduated pressure. The compression is strongest at the ankle and gradually decreases up the leg, which helps prevent blood from pooling in the lower extremities and supports proper venous function. This graduated pressure works with your body’s natural mechanisms to encourage blood flow against gravity, promoting healthier circulation throughout your lower limbs and reducing the workload on your venous system.
At DailyNergy, our compression socks are designed to provide relief from various conditions including leg swelling, varicose veins, and general fatigue. These specially engineered garments work by promoting better blood flow from your lower extremities back to your heart, helping to reduce swelling and discomfort throughout the day. The medical-grade elasticity in our products ensures consistent pressure distribution that adapts to your unique leg contours while maintaining therapeutic compression levels during various activities.
The primary benefits of compression socks include:
- Improved blood circulation in the legs by enhancing venous return to the heart
- Reduced swelling in feet, ankles, and calves through controlled pressure that prevents fluid accumulation
- Prevention of blood clots, especially during long periods of inactivity such as long-haul flights or hospital stays
- Relief from symptoms of varicose veins by supporting vein walls and reducing venous pressure
- Decreased leg fatigue and discomfort, particularly for those who stand for extended periods in occupations like healthcare, retail, or service industries
- Enhanced athletic performance and recovery by improving oxygen delivery to muscles and reducing lactic acid buildup
- Management of certain medical conditions like lymphedema, chronic venous insufficiency, and post-thrombotic syndrome
While compression socks offer numerous benefits, the question of whether they should be worn continuously, 24 hours a day, 7 days a week, requires careful consideration. Let’s explore the recommended usage patterns and potential risks of continuous wear to help you make an informed decision about your compression therapy regimen based on your specific health needs and lifestyle factors.
The Standard Recommendation: When to Wear Compression Socks
For most people, compression socks are not designed for continuous 24/7 wear. The standard recommendation is to wear them during waking hours, typically for 8-10 hours per day, and remove them at night when sleeping. This approach allows your skin to breathe and recover while still providing the therapeutic benefits during your most active hours. Healthcare professionals generally advise this schedule because it balances the circulatory benefits of compression with the need to give your skin and tissues periodic relief from constant pressure.
The optimal time to put on compression socks is in the morning, immediately after waking up and before getting out of bed. This is when your legs are least swollen, making it easier to apply the socks and ensuring maximum benefit throughout the day. Our DailyNergy Compression Socks Size L and other sizes are designed for comfortable all-day wear during your active hours. The specialized weave and fabric composition of our socks maintain consistent pressure while allowing sufficient airflow to keep your legs comfortable throughout extended periods of wear.
Here’s a general guideline for when to wear compression socks:
- During the day while you’re active or sitting for long periods, such as at a desk job or during travel
- When traveling, especially during long flights where cabin pressure and limited movement increase swelling risk
- While exercising, if recommended by your healthcare provider, to improve performance and reduce recovery time
- During pregnancy to help with swelling and prevent varicose veins, particularly in the second and third trimesters
- After surgery, as directed by your medical team, to prevent post-operative complications like deep vein thrombosis
- For specific occupations requiring prolonged standing or sitting, such as nurses, retail workers, or office professionals
- During long periods of immobility, such as when recovering from an injury or illness that limits movement
Most healthcare professionals recommend removing compression socks before going to bed to allow your skin to breathe and recover. This overnight break helps maintain skin integrity and reduces the risk of complications from continuous pressure. However, there are exceptions to this rule, which we’ll discuss in the next section. It’s important to note that the appropriate wearing schedule may vary based on individual health conditions, lifestyle factors, and the specific recommendations of your healthcare provider.
Medical Exceptions: When 24/7 Wear May Be Prescribed
While continuous 24/7 wear is not the standard recommendation, there are specific medical conditions and circumstances where healthcare providers might prescribe around-the-clock compression therapy. In these cases, the benefits of continuous compression outweigh the potential risks, and special considerations are typically made to minimize complications. Your healthcare provider will carefully evaluate your specific situation, considering factors such as your overall health, the severity of your condition, and your body’s response to compression therapy.
Situations where 24/7 compression sock wear might be recommended include:
1. Post-surgical recovery: After certain surgeries, especially vascular or orthopedic procedures, continuous compression may be prescribed to prevent blood clots and reduce swelling. Our guide on wearing compression socks after knee surgery provides detailed information on this topic. Surgeons often prescribe 24-hour compression during the initial recovery phase to minimize the risk of deep vein thrombosis and promote optimal healing by controlling post-operative edema.
2. Deep vein thrombosis (DVT) treatment: For patients with a history of blood clots or those at high risk, continuous compression may be necessary to prevent clot formation. The consistent pressure helps maintain proper blood flow in the deep veins, reducing the risk of dangerous clot development. In these cases, healthcare providers may recommend specialized compression garments designed specifically for overnight wear that provide therapeutic pressure while minimizing discomfort during sleep.
3. Severe venous insufficiency: In cases of advanced venous disease, 24/7 compression might be required to manage symptoms and prevent complications. When the venous valves are severely compromised, continuous external support helps maintain proper fluid balance and prevents the progression of complications such as venous stasis ulcers, which can be difficult to heal once developed.
4. Lymphedema management: Patients with lymphedema often need continuous compression to control swelling and prevent infection. The lymphatic system relies on external pressure to help move lymph fluid when its natural drainage mechanisms are compromised. Without consistent compression, rapid fluid accumulation can occur, potentially leading to increased risk of cellulitis and other complications.
5. Bedridden patients: Those confined to bed may need constant compression to prevent complications associated with immobility. The lack of muscle contraction in bedridden individuals significantly reduces natural venous return, making external compression crucial for preventing blood stasis and subsequent complications like pressure ulcers and thrombosis.
If your healthcare provider has recommended 24/7 compression therapy, they will likely prescribe specialized garments designed for overnight wear, which may differ from standard daytime compression socks. These nighttime compression options often feature different materials, compression gradients, or design elements to enhance comfort while maintaining therapeutic pressure. Always follow your healthcare provider’s specific instructions regarding duration and type of compression, and report any unusual symptoms or discomfort promptly.
Potential Risks of Wearing Compression Socks 24/7
While compression socks are generally safe when used as directed, wearing them continuously without proper breaks can pose certain risks to your skin and circulation. Understanding these potential complications is essential for making informed decisions about your compression therapy regimen, especially if you’re considering extended wear periods or have been prescribed continuous compression by your healthcare provider.
Potential complications from continuous wear include:
1. Skin irritation and breakdown: Prolonged pressure and moisture can lead to skin issues, including rashes, irritation, and in severe cases, pressure ulcers. The constant pressure combined with heat and moisture creates an environment where the skin’s protective barrier can become compromised. This is particularly concerning for individuals with sensitive skin, diabetes, or peripheral neuropathy who may have reduced sensation and might not notice early warning signs of skin damage.
2. Reduced circulation: Ironically, compression socks that are too tight or worn for too long can actually impede circulation rather than improve it, especially if they bunch up or roll down. When compression garments create localized areas of excessive pressure, they can restrict arterial flow while attempting to support venous return. This paradoxical effect is more common with improperly fitted garments or those that have lost their elasticity through extended wear or improper care.
3. Bacterial or fungal infections: Continuous wear creates a warm, moist environment that can promote the growth of bacteria and fungi, potentially leading to infections. The limited airflow and accumulated perspiration provide ideal conditions for microorganisms to thrive, particularly in the spaces between toes and in skin folds. Individuals with compromised immune systems or diabetes face elevated risks from these infections, which can become serious if not promptly addressed.
4. Nerve compression: Extended wear of tight compression garments can sometimes lead to nerve compression, causing tingling, numbness, or pain. Peripheral nerves, particularly those that run close to the skin’s surface, can become irritated or compressed by constant pressure. This neuropathic discomfort may begin subtly but can progress to more significant symptoms if the compression is not adjusted or temporarily discontinued.
5. Dependency: In some cases, continuous wear may lead to a dependency where your veins rely on the external compression, potentially weakening over time. When the body becomes accustomed to external support, the natural muscular and vascular mechanisms that promote venous return might become less efficient. This potential physiological adaptation underscores the importance of balancing compression therapy with appropriate physical activity and periodic breaks when medically appropriate.
6. Temperature regulation issues: Continuous compression can interfere with your body’s natural temperature regulation in the lower extremities, potentially causing discomfort in varying environmental conditions. The additional layer of tight fabric may increase heat retention during warm weather or activities, while the compression itself might reduce natural warming circulation in colder conditions.
To minimize these risks while still enjoying the benefits of DailyNergy compression socks, it’s important to follow proper wear and care guidelines, which we’ll discuss next. Regular monitoring of skin condition, proper hygiene practices, and adherence to your healthcare provider’s recommendations can significantly reduce the likelihood of experiencing adverse effects from compression therapy.
Proper Application and Removal for Optimal Benefits
The effectiveness and safety of compression socks largely depend on proper application and removal techniques. Incorrect application can reduce the benefits and potentially cause discomfort or harm. Taking the time to learn and practice these techniques ensures you’ll receive the maximum therapeutic value from your compression garments while minimizing the risk of complications, especially if you’re using them for extended periods.
How to Apply Compression Socks Correctly:
1. Apply to clean, dry skin: Make sure your legs and feet are completely dry to prevent skin irritation. Applying a small amount of talcum powder or cornstarch can help absorb moisture and make application easier, especially in hot weather or if you tend to perspire heavily.
2. Apply first thing in the morning: Put on your compression socks before getting out of bed when your legs are least swollen. Overnight, while you’re horizontal, fluid that may have accumulated during the previous day has a chance to redistribute, making morning the optimal time to begin compression therapy for maximum effectiveness.
3. Turn the sock inside out to the heel: This makes it easier to position the sock correctly. Create a “pocket” by turning the sock inside out up to the heel area, which allows you to position your foot properly before rolling the sock up your leg. This technique significantly reduces the struggle often associated with putting on compression garments.
4. Position the sock properly: Ensure the heel is in the right place and the sock is not twisted. Proper alignment of the garment’s anatomical features with your own anatomy is crucial for both comfort and therapeutic effectiveness. Misaligned compression socks can create pressure points or areas of inadequate compression.
5. Gradually pull up the sock: Work it up your leg evenly without letting it bunch or roll. Use the palms of your hands rather than just your fingertips to distribute the force evenly as you work the sock upward. Take your time with this step to ensure the compression gradient remains properly distributed.
6. Ensure proper fit: The sock should feel snug but not painfully tight. There should be no bunching or wrinkling. Once applied, run your hands over the entire surface to smooth out any remaining wrinkles or folds. The top band should sit flat against your skin without cutting in or rolling down.
7. Check circulation: After application, ensure your toes are not discolored, numb, or tingling, which could indicate the compression is too tight. You should be able to wiggle your toes freely, and the sock should not cause pain or discomfort at any point along your leg.
How to Remove Compression Socks:
1. Peel the sock down: Start at the top and gently roll it down. Fold the top band over and continue to work it downward in sections rather than attempting to remove the entire sock at once. This methodical approach prevents unnecessary strain on the fabric and your skin.
2. Don’t pull from the toe: This can damage the sock and make removal more difficult. Pulling from the toe end creates excessive strain on the fabric and can distort the compression gradient over time, reducing the therapeutic effectiveness and lifespan of the garment.
3. Use rubber gloves if needed: These can provide better grip for easier removal. The improved traction from rubber gloves is particularly helpful for individuals with limited hand strength or arthritis, making the removal process less strenuous and reducing the risk of skin tears from forceful pulling.
4. Consider using a removal aid: If you have difficulty removing your socks, specialized devices are available. These tools, which include sock sliders and donning/doffing aids, can be invaluable for maintaining independence with compression therapy, especially for elderly individuals or those with mobility limitations.
5. Inspect your skin after removal: Check for any signs of irritation, pressure marks, or discoloration. This daily skin check is an important safety practice, particularly if you’re using compression therapy for extended periods or have conditions that affect skin integrity or sensation.
For those with limited mobility or strength, applying and removing compression socks can be challenging. In such cases, consider asking for help or using application aids specifically designed for compression garments. Many home health suppliers and medical supply stores offer a variety of tools to make compression therapy more accessible for individuals with physical limitations.
The Importance of Proper Sizing and Compression Levels
Choosing the right size and compression level is crucial for both comfort and effectiveness. Compression socks that are too tight can cause harm, while those that are too loose won’t provide the intended benefits. The therapeutic value of compression therapy is directly related to applying the correct amount of pressure to specific areas of your legs, which can only be achieved with properly sized garments that deliver appropriate compression levels for your particular condition.
Compression Levels Explained:
Compression socks are measured in millimeters of mercury (mmHg), indicating the amount of pressure applied. Understanding these different levels helps you select the appropriate compression for your specific needs:
- 8-15 mmHg (Mild): For everyday wear, travel, and minor swelling. This entry-level compression provides gentle support suitable for healthy individuals seeking preventive benefits during long periods of sitting or standing. These are often recommended for first-time compression sock users to help them adjust to the sensation of compression therapy.
- 15-20 mmHg (Moderate): For long periods of standing, pregnancy, and minor varicose veins. This level offers more substantial support without being overly restrictive, making it ideal for individuals experiencing mild symptoms or those with occupations requiring prolonged standing, such as teachers, retail workers, or healthcare professionals.
- 20-30 mmHg (Firm): For moderate to severe varicose veins, post-sclerotherapy, and preventing DVT. This medical-grade compression is often prescribed for specific conditions and provides significant therapeutic pressure. It’s commonly recommended for post-surgical recovery, managing moderate edema, and supporting compromised venous function.
- 30-40 mmHg (Extra Firm): For severe varicose veins, lymphedema, and severe edema. This high level of compression delivers powerful support for serious venous and lymphatic conditions. Due to the strength of compression, proper fitting by a trained professional is particularly important at this level to ensure safety and effectiveness.
- 40+ mmHg (Medical Grade): Usually prescribed for severe conditions and requires a doctor’s prescription. This highest level of compression is reserved for managing complex medical conditions like severe post-thrombotic syndrome, advanced lymphedema, or venous ulcers. These garments should only be used under close medical supervision due to their potential to restrict arterial flow if improperly fitted.
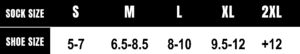
At DailyNergy, we offer a range of sizes to ensure a perfect fit for everyone. From Size S to Size 2XL, our compression socks are designed to provide optimal support without compromising comfort. Our comprehensive sizing system accommodates various leg dimensions, ensuring that users of all body types can find compression garments that deliver the proper therapeutic pressure while remaining comfortable for extended wear.
How to Measure for Proper Sizing:
1. Measure in the morning: Take measurements when your legs are least swollen, typically first thing in the morning before getting out of bed. This provides the most accurate baseline dimensions for selecting compression garments that will fit properly throughout the day, even as normal fluid fluctuations occur.
2. Ankle circumference: Measure around the narrowest part of your ankle, just above the ankle bone. This measurement is particularly critical as it’s where compression should be strongest in graduated compression garments. Be sure to keep the measuring tape snug but not tight, and measure both ankles as there may be slight differences between them.
3. Calf circumference: Measure the widest part of your calf. For most people, this is approximately halfway between the ankle and knee. Take this measurement while seated with your feet flat on the floor and knees bent at a 90-degree angle to ensure consistency and accuracy.
4. Leg length: For knee-high socks, measure from the floor to the bend of your knee. For thigh-high options, continue measuring to the desired height. This dimension ensures that your compression garments will reach the appropriate level on your leg without being too short (reducing effectiveness) or too long (causing bunching).
5. Thigh circumference: If selecting thigh-high compression stockings, measure the circumference at the widest part of your thigh, typically just below the gluteal fold. This measurement helps ensure proper fit and prevents the top band from rolling down or creating a tourniquet effect.
Using our sizing chart, you can find the perfect fit for your needs. Remember, compression socks should feel snug but not painful. If you experience numbness, tingling, or severe discomfort, the size or compression level may not be right for you. When in doubt, consult with a healthcare professional or compression specialist who can provide personalized guidance based on your specific measurements and medical requirements.
Alternatives to 24/7 Wear: Balancing Compression Benefits
If you’re considering 24/7 compression but haven’t been specifically directed to do so by a healthcare provider, there are alternative approaches that can provide benefits while minimizing risks. These strategies allow you to maintain good circulation and manage symptoms while giving your skin and tissues necessary breaks from constant pressure. Finding the right balance is key to sustainable, long-term compression therapy that supports your health without creating new problems.
Balanced Compression Strategies:
1. Daytime wear with nighttime elevation: Wear compression socks during the day and elevate your legs at night to continue promoting good circulation. Elevating your legs above heart level for 20-30 minutes before bed helps naturally reduce swelling by using gravity to assist venous return. This combination approach provides therapeutic pressure during active hours while allowing your skin to rest overnight without sacrificing circulatory benefits.
2. Alternating compression garments: Use different types of compression garments for different activities. For example, DailyNergy compression socks during the day and looser sleep compression garments at night if prescribed. This rotation allows you to maintain appropriate compression levels for various activities while distributing pressure to different areas of your legs, reducing the risk of pressure-related complications at any single point.
3. Targeted compression: Use knee compression sleeves or other targeted compression products for specific areas rather than full leg compression when appropriate. This focused approach can address localized issues—such as knee swelling or calf discomfort—without subjecting your entire leg to compression. Targeted products are often easier to apply and remove, making them more accessible for intermittent use throughout the day.
4. Scheduled breaks: If you need extended compression, work with your healthcare provider to establish a schedule that includes short breaks to check skin condition and allow for cleaning. These planned intervals—perhaps 30 minutes in the morning and evening—provide opportunities to inspect your skin, apply moisturizer if needed, and give your tissues temporary relief from constant pressure while still maintaining the overall benefits of compression therapy.
5. Complementary therapies: Combine compression therapy with other approaches such as exercise, elevation, and proper hydration for maximum benefit. Regular ankle pumps, calf raises, and walking help activate your calf muscle pump—the body’s natural mechanism for promoting venous return. Staying well-hydrated improves blood viscosity, making circulation more efficient, while limiting salt intake can reduce fluid retention that contributes to swelling.
6. Progressive compression schedule: If you’re new to compression therapy, start with shorter wearing periods and gradually increase duration as your body adapts. Beginning with 2-4 hours and adding an hour each day until reaching the recommended wearing time allows your skin and tissues to adjust to the pressure while minimizing discomfort and potential complications.
7. Activity-based compression: Reserve your highest compression levels for periods of greatest need, such as during exercise, long periods of sitting or standing, or air travel. Lower compression or no compression might be appropriate during rest periods or activities with frequent position changes that naturally promote circulation.
Our DailyNergy Knee Sleeve products offer targeted compression for joint pain relief and improved circulation around the knee area, providing an excellent alternative or complement to full-leg compression socks. These specialized sleeves deliver therapeutic pressure precisely where needed while allowing other areas to remain unrestricted, making them ideal for activities where full leg compression might be uncomfortable or impractical.
Special Considerations for Nighttime Wear
If your healthcare provider has recommended wearing compression socks during sleep, or if you’re experiencing symptoms that might benefit from nighttime compression, there are special considerations to keep in mind. Nighttime compression presents unique challenges and opportunities that differ from daytime wear, requiring specific approaches to ensure both comfort and therapeutic effectiveness while you sleep.
Benefits of Nighttime Compression:
1. Continued circulation support: For some conditions, maintaining compression overnight can help prevent fluid buildup. While you’re horizontal during sleep, gravity’s effect on fluid distribution changes, but compression can still help maintain proper venous and lymphatic flow, preventing the morning swelling that many people with circulatory issues experience.
2. Symptom management: Nighttime compression may help manage restless legs syndrome or night cramps, as discussed in our article about how compression socks help with restless legs. The gentle pressure can help reduce the uncomfortable sensations that trigger movement urges in RLS and may stabilize muscle activity that contributes to nocturnal cramping.
3. Post-surgical recovery: Following certain procedures, continuous compression may be necessary to prevent complications. During the critical early recovery period after vascular or orthopedic surgeries, the risk of blood clot formation remains high even during sleep. Maintaining therapeutic compression helps mitigate this risk while also controlling post-operative swelling that can impede healing.
4. Consistency in therapy: For conditions like lymphedema, uninterrupted compression may provide better long-term management by preventing the reaccumulation of fluid that can occur during periods without compression. The lymphatic system doesn’t have a central pump like the circulatory system, making external compression particularly important for maintaining proper lymph flow.
5. Enhanced recovery for athletes: Some evidence suggests that nighttime compression may improve recovery processes by supporting circulation during the body’s natural repair cycle. This can be particularly beneficial for competitive athletes or those engaged in intensive training programs where optimizing recovery is crucial for performance.
Recommendations for Nighttime Wear:
1. Use lower compression levels: If wearing compression socks at night, consider a lower compression level than what you use during the day. The horizontal position during sleep naturally reduces gravitational pressure on your venous system, so less external compression is typically needed to achieve therapeutic benefits. Many people find that 15-20 mmHg is sufficient for nighttime use, even if they require stronger compression during daytime activities.
2. Choose specific nighttime garments: Some compression garments are designed specifically for nighttime wear, offering more comfort while sleeping. These specialized products often feature softer fabrics, fewer seams, and modified compression gradients that accommodate the different physiological demands of the recumbent position. They may also incorporate design elements that prevent bunching or rolling during the natural movements that occur during sleep.
3. Monitor skin condition: Check your skin regularly for any signs of irritation or pressure points. Establish a routine of morning and evening skin inspections, paying particular attention to bony prominences, joints, and areas where the compression garment might fold or wrinkle. Early detection of skin changes allows for prompt intervention before minor irritation develops into more significant problems.
4. Keep extra pairs handy: If you’re wearing compression socks 24/7, having multiple pairs allows you to change them regularly for hygiene purposes. Maintaining at least three pairs enables you to rotate them while allowing sufficient time for washing and complete drying between uses. This rotation system helps preserve the elastic properties of the garments while ensuring you always have clean compression socks available.
5. Consider specialized fabrics: Look for moisture-wicking materials that can help keep skin dry and comfortable overnight. Advanced technical fabrics can draw perspiration away from your skin while allowing sufficient airflow to prevent the warm, moist environment that promotes skin breakdown and fungal growth. Some nighttime compression garments also incorporate antimicrobial treatments for additional protection.
6. Adjust room temperature: If wearing compression garments at night, you might need to adjust your sleeping environment to prevent overheating. Lowering the room temperature slightly or using breathable bedding can help compensate for the additional warmth created by compression garments, improving overall sleep quality and comfort.
Remember, nighttime wear should generally only be undertaken with specific medical guidance. If you’re experiencing symptoms that make you consider 24/7 compression, consult with a healthcare provider first. They can help determine whether continuous compression is appropriate for your condition and recommend the safest, most effective approach for your individual needs.
Caring for Your Compression Socks to Extend Their Life
Proper care of your compression socks is essential, especially if you’re wearing them frequently or continuously. Well-maintained compression garments will provide consistent pressure and last longer. The specialized elastic fibers that create therapeutic compression require specific care practices to maintain their integrity and effectiveness over time. Investing a little extra attention in the maintenance of your compression socks ultimately saves money by extending their useful life while ensuring they continue to deliver the intended medical benefits.
Washing and Drying Instructions:
1. Hand wash when possible: Gentle hand washing in lukewarm water with mild soap is ideal. This method minimizes stress on the elastic fibers that provide compression. Fill a basin with lukewarm water (not hot, which can damage elasticity), add a small amount of mild detergent specifically formulated for delicate fabrics, and gently agitate the socks for a few minutes before rinsing thoroughly.
2. If machine washing: Use a gentle cycle and place socks in a mesh laundry bag to protect them. This extra layer of protection prevents the compression garments from becoming entangled with other items or caught in machine components. Always fasten any closures before washing to prevent them from catching on other items and potentially damaging the fabric.
3. Avoid harsh detergents: Do not use bleach, fabric softeners, or harsh chemicals that can break down the elastic fibers. These aggressive substances can degrade the specialized elastomeric materials that create the compression gradient. Similarly, avoid detergents with enzymes or brighteners, which can be too harsh for the technical fabrics used in compression garments.
4. Air dry flat: Hang drying can stretch the garment, while machine drying can damage the elastic. Lay your compression socks on a clean, dry towel away from direct sunlight and heat sources, which can cause the elastic to deteriorate prematurely. Reshape the socks while damp to maintain their proper form and compression gradient during drying.
5. Avoid wringing: Gently press water out rather than twisting or wringing, which can damage the compression fibers. Place the wet garments between clean towels and press to remove excess moisture before laying them flat to dry. This technique preserves the elastic properties while speeding up the drying process.
6. Never iron compression garments: The heat from an iron can permanently damage the elastic fibers that provide therapeutic compression. If your socks become wrinkled, proper storage and handling should eliminate the issue without requiring ironing. If absolutely necessary, use the lowest heat setting and place a cloth barrier between the iron and the compression garment.
Rotation and Replacement:
1. Have multiple pairs: If you wear compression socks daily or continuously, have at least 2-3 pairs to rotate through. Our 3-pair bundles offer excellent value and convenience. This rotation system allows each pair sufficient time to fully dry between wearings and distributes wear evenly across multiple garments, extending the overall lifespan of your compression sock collection.
2. Replace regularly: Most compression socks need to be replaced every 3-6 months with regular wear, as they gradually lose their elasticity. Even with perfect care, the constant stretching and compression of the specialized fibers eventually causes them to lose their ability to deliver consistent therapeutic pressure. Establishing a regular replacement schedule ensures you’re always receiving the intended medical benefits.
3. Watch for signs of wear: Stretched-out areas, thinning fabric, or decreased compression are signs it’s time for a replacement. You might notice that the socks feel looser, take longer to put on, or no longer provide the same level of symptom relief. Any visible damage such as runs, holes, or permanent creases indicates that the garment can no longer deliver proper therapeutic compression.
4. Check the fit periodically: If your weight fluctuates or your condition changes, you may need to reassess your size. Even modest weight changes can affect the circumference of your ankles and calves, potentially altering the fit and effectiveness of your compression garments. Similarly, changes in your medical condition might require adjustments to your compression level or garment style.
5. Store properly: Between wearings, store your compression socks in a cool, dry place away from direct sunlight. Avoid folding them in ways that create sharp creases, which can weaken the elastic fibers at the fold points. Instead, roll them loosely or lay them flat in a drawer dedicated to your compression garments.
With proper care, your DailyNergy compression socks will maintain their therapeutic benefits longer, providing consistent support whether you’re wearing them for specific activities or for extended periods as directed by your healthcare provider. The investment in proper maintenance pays dividends through improved comfort, extended product lifespan, and consistent therapeutic benefits throughout the life of the garment.
When to Consult a Healthcare Professional
While compression socks are available over the counter, there are situations where professional medical advice is necessary, especially when considering 24/7 wear. Compression therapy, while generally safe, represents a medical intervention that can have significant impacts on your circulatory system and overall health. Knowing when to seek professional guidance ensures you’ll receive maximum benefits while avoiding potential complications.
Seek Medical Advice If:
1. You have underlying health conditions: Conditions such as diabetes, arterial disease, or skin disorders may affect whether compression therapy is appropriate. These conditions can alter peripheral circulation and skin integrity, potentially increasing the risks associated with compression therapy. A healthcare provider can evaluate your specific situation and recommend appropriate modifications to standard compression protocols.
2. You’re considering 24/7 wear: Always consult a healthcare provider before wearing compression socks around the clock. Continuous compression represents a significant intervention that requires professional assessment of both benefits and risks. Your provider can determine whether your specific condition warrants 24-hour compression and can recommend appropriate products and monitoring protocols.
3. You experience new or worsening symptoms: Pain, numbness, tingling, color changes in your skin, or increased swelling while wearing compression socks warrants medical attention. These symptoms might indicate that your compression level is inappropriate, your garments don’t fit correctly, or that you have an underlying condition requiring different management approaches.
4. You have difficulty putting on or taking off the socks: This might indicate they’re too tight or that you need a different type of compression garment. Excessive difficulty with application could lead to improper use or abandonment of therapy. Healthcare providers can recommend alternative compression options or assistive devices that make application and removal easier.
5. You develop skin irritation or breakdown: Any skin changes should be evaluated promptly. Redness, rashes, blisters, or open areas require immediate attention to prevent infection and more serious complications. Your provider may recommend temporary discontinuation of compression therapy, alternative garment materials, or adjunctive skin care practices.
6. You’re pregnant: While compression socks are often beneficial during pregnancy, the changing physiology and potential complications require professional oversight. A healthcare provider can help determine appropriate compression levels as your pregnancy progresses and monitor for pregnancy-specific circulatory concerns.
7. You’ve recently undergone surgery: Post-surgical compression needs are highly specific to the procedure performed and your individual risk factors. Your surgical team should provide detailed guidance on compression therapy as part of your recovery plan, including when to start, what type to use, and how long to continue.
What to Discuss With Your Healthcare Provider:
1. Your specific condition and symptoms: Be detailed about what you’re experiencing and when. Note whether symptoms occur at particular times of day, after specific activities, or in certain positions. This temporal information helps your provider understand the nature of your circulatory issues and recommend appropriate interventions.
2. Your daily activities: Discuss your lifestyle, occupation, and activity level. These factors significantly influence both your circulatory needs and the practical aspects of implementing compression therapy. A construction worker who stands all day has different requirements than an office worker or a competitive athlete.
3. Your current compression routine: If you’re already using compression products, share details about the type, compression level, and wearing schedule. Bring your current garments to your appointment if possible, as this allows your provider to evaluate their condition, fit, and appropriateness for your needs.
4. Any difficulties or concerns: Be honest about any challenges you’re facing with your current compression therapy. Whether it’s physical discomfort, practical application issues, or concerns about appearance, your provider needs this information to help develop sustainable solutions that you’ll be able to maintain long-term.
5. Your goals for compression therapy: Clarify what you hope to achieve with compression socks. Whether you’re seeking symptom relief, prevention of complications, improved athletic performance,